Macular Degeneration and Nutrition Center
“Age-related macular degeneration affects more than 1.75 million individuals in the United States. Owing to the rapid aging of the US population, this number will increase to almost 3 million by 2020.”
 Macular degeneration is the leading cause of severe vision loss in people over age 60. It occurs when the small central portion of the retina, known as the macula, deteriorates over time. The retina is the light-sensing nerve tissue at the back of the eye. Because the disease develops as a person ages, it is often referred to as age-related macular degeneration (AMD). Although macular degeneration is almost never a totally blinding condition, it can be a source of significant visual disability for patients and their families.
Macular degeneration is the leading cause of severe vision loss in people over age 60. It occurs when the small central portion of the retina, known as the macula, deteriorates over time. The retina is the light-sensing nerve tissue at the back of the eye. Because the disease develops as a person ages, it is often referred to as age-related macular degeneration (AMD). Although macular degeneration is almost never a totally blinding condition, it can be a source of significant visual disability for patients and their families.
There are two main types of age-related macular degeneration:
Dry form. The “dry” form of macular degeneration is characterized by the presence of yellow deposits, called drusen, in the macula. A few small drusen may not cause changes in vision; however, as they grow in size and increase in number, they may lead to a dimming or distortion of vision that people find most noticeable when they read. In more advanced stages of dry macular degeneration, there is also a thinning of the light-sensitive layer of cells in the macula leading to atrophy, or tissue death. In the atrophic form of dry macular degeneration, patients may have blind spots in the center of their vision. In the advanced stages, patients lose central vision.
Wet form. The “wet” form of macular degeneration is characterized by the growth of abnormal blood vessels from the choroid underneath the macula. This is called choroidal neovascularization. These blood vessels leak blood and fluid into the retina, causing distortion of vision that makes straight lines look wavy, as well as blind spots and loss of central vision. These abnormal blood vessels eventually scar, leading to permanent loss of central vision.
Most patients with macular degeneration have the dry form of the disease and will not lose their entire central vision. However, the dry form of macular degeneration can lead to the wet form. Although only about 10% of people with macular degeneration develop the wet form, they make up the majority of those who experience serious vision loss from the disease.
It is very important for people with macular degeneration to monitor their eyesight carefully and see their eye doctor on a regular basis.
What Are the Risk Factors for Macular Degeneration?
As the name suggests, age-related macular degeneration is more common in older adults. In fact, it is the leading cause of severe vision loss in adults over age 60.
Macular degeneration may be hereditary, meaning it can be passed on from parents to children. If someone in your family has or had the condition you may be at higher risk for developing macular degeneration. Talk to your eye doctor about your individual risk.
- Family History of Age-Related Macular Degeneration
- Smoking
- Obesity
- Hypertension
- Hypercholesterolemia
- UV Radiation Exposure
- Poor Diet
What Are the Symptoms of Macular Degeneration?
In its early stages, macular degeneration may not have symptoms and may be unrecognized until it progresses or affects both eyes. The first sign of macular degeneration is usually a dim, blurry spot in the middle of your vision. This spot may get bigger or darker over time.
Symptoms of macular degeneration include:
- Dark, blurry areas in the center of vision
- Diminished or changed color perception
- Difficulty seeing in low light conditions
If you experience any of these symptoms, see your ophthalmologist as soon as possible.
How Is Macular Degeneration Diagnosed?
Age-related macular degeneration can be detected in a routine eye exam. One of the most common early signs of macular degeneration is the presence of drusen — tiny yellow deposits under the retina. Your doctor can see these when examining your eyes. Your doctor may also ask you to look at an Amsler grid — a pattern of straight lines that resemble a checkerboard. Some of the straight lines may appear wavy to you, or you may notice that some of the lines are missing. These can also be signs of macular degeneration.
If your doctor detects age-related macular degeneration, you may have a procedure called angiography or an OCT. In angiography, a dye is injected into a vein in the arm. Photographs are taken as the dye reaches the eye and flows through the blood vessels of the retina. If there are new vessels or vessels leaking fluid or blood in the macula, the photographs will show their exact location and type. OCT is able to see fluid or blood underneath the retina without using dye.
Early detection of age-related macular degeneration is very important because there are treatments that can delay or reduce the severity of the disease.
What Treatments Are Available for Macular Degeneration?
There is currently no cure for macular degeneration, but treatments may prevent severe vision loss or slow the progression of the disease considerably. Several options are available, including:
Anti-angiogenesis drugs. These medications (Avastin, Lucentis, Macugen) block the development of new blood vessels and leakage from the abnormal vessels within the eye that cause wet macular degeneration. This treatment has been a major change in the treatment of this condition and many patients have actually regained vision that was lost. The treatment may need to be repeated during follow-up visits.
Vitamins. A large study performed by the National Eye Institute of the National Institutes of Health, called AREDS (Age-Related Eye Disease Study), showed that for certain individuals, vitamins C, E, beta-carotene, zinc and copper can decrease the risk of vision loss in patients with intermediate to advanced dry macular degeneration. Ask your eye doctor if these vitamin supplements will benefit you before taking them and see our link below to determine which antioxidant supplement may be right for you.
Laser therapy. High-energy laser light can sometimes be used to destroy actively growing abnormal blood vessels that occur in macular degeneration.
Low vision aids. Devices that have special lenses or electronic systems that produce enlarged images of nearby objects. They help people who have vision loss from macular degeneration make the most of their remaining vision.
What Is the Outlook for People With Macular Degeneration?
People rarely lose all of their vision from age-related macular degeneration. They may have poor central vision, but they are still able to perform many normal daily activities.
The wet form of macular degeneration is a leading cause of irreversible vision loss. When both eyes are affected, you may experience a significant decrease in your quality of life.
The dry form of age-related macular degeneration is much more common and tends to progress more slowly, allowing you to keep most of your central and peripheral vision.
Unfortunately, even after wet macular degeneration treatment, the condition can recur. Because of this, individuals with macular degeneration must test their own vision regularly and follow the recommendations of their ophthalmologist. Successful and timely treatment will slow the rate of vision loss and often improve vision.
How important is nutrition in protecting eye health?
Cumulative oxidative damage has been implicated in the pathogenesis of age-related macular changes.1,2 Emerging scientific data suggest that high concentrations of key nutrients are critical to protecting the eye against oxidative stress and maintaining optimal function. Ensuring proper nutrition is particularly important during aging, to offset age-related decline of key nutrients.
Oxidative stress and the eye
 The eye is uniquely conducive to the generation of reactive oxygen intermediates and therefore highly susceptible to oxidative stress.1,3 The retina is particularly vulnerable.1,3 The retina has a rich oxygen supply, with an oxygen requirement almost as high as that of arterial blood. (3) Oxygen consumption in the retina is greater than in any other tissue. (1)
The eye is uniquely conducive to the generation of reactive oxygen intermediates and therefore highly susceptible to oxidative stress.1,3 The retina is particularly vulnerable.1,3 The retina has a rich oxygen supply, with an oxygen requirement almost as high as that of arterial blood. (3) Oxygen consumption in the retina is greater than in any other tissue. (1)
The antioxidant system in the eye includes antioxidant enzymes (for example, catalase and superoxide dismutase), vitamins C and E, zinc, and the macular pigment. (1,4-6)
Omega-3 fatty acids in the retina also participate in the oxidative stress response and are important in protecting retinal function. (7-12)
The macular pigment is composed of the dietary carotenoids lutein, zeaxanthin, and meso-zeaxanthin, a metabolite of lutein. (1,3) These carotenoids protect against oxidative stress in two ways (1,13) :
- By filtering potentially damaging blue light, thereby reducing photo-oxidation
- By quenching reactive oxygen intermediates
The omega-3 fatty acid docosahexaenoic acid (DHA) has a well-established role in retinal function. (9) DHA is found at high concentrations in rod outer segments of the retina. (10,11) As photoreceptor outer segments are continuously shed, adequate DHA may be critical to replenish levels. (11) Eicosapentaenoic acid (EPA) is another important long-chain polyunsaturated omega-3 fatty acid in that it serves as a substrate for DHA biosynthesis and also may have anti-inflammatory effects. (12)
Factors associated with decline in the protective antioxidant system
Aging
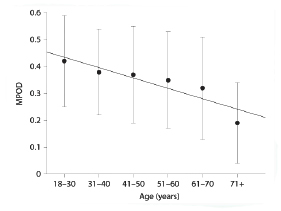 Aging is associated with a decline in macular pigment. (3,15,16) A variety of possible factors may contribute to this decline, including changes in dietary intake of lutein and zeaxanthin, age-related changes in the absorption or distribution of the macular carotenoids, and/or excessive depletion due to an age-related increase in oxidative stress. (15)
Aging is associated with a decline in macular pigment. (3,15,16) A variety of possible factors may contribute to this decline, including changes in dietary intake of lutein and zeaxanthin, age-related changes in the absorption or distribution of the macular carotenoids, and/or excessive depletion due to an age-related increase in oxidative stress. (15)
Age-related decline in macular pigment optical density (MPOD) (15)
Smoking
History of smoking is associated with reduced macular pigment (as evidenced by lower MPOD), perhaps due to a higher oxidant load that could increase turnover of carotenoids. (3,15,16)
Genetics
Factors associated with lower macular pigment optical density (3,15,16,20-22)
- Aging
- Genetics
- Diet
- Blue to gray iris color
- Smoking
- ApoE genotype
Strategies to increase macular pigment
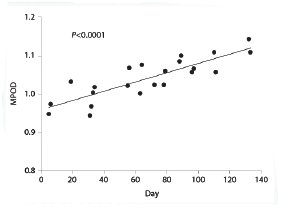 Several studies of adopting a diet rich in lutein- and zeaxanthin-containing foods have demonstrated a positive effect on macular pigment. (23-26) Similarly, supplementation with lutein and zeaxanthin has been demonstrated to significantly increase macular pigment. (13,27-29)
Several studies of adopting a diet rich in lutein- and zeaxanthin-containing foods have demonstrated a positive effect on macular pigment. (23-26) Similarly, supplementation with lutein and zeaxanthin has been demonstrated to significantly increase macular pigment. (13,27-29)
Increase in macular pigment in an individual receiving lutein supplementation (27)
Adapted with permission from Bone et al. (27)
In this study, lutein was dosed at 5 mg, 10 mg, and 20 mg daily. All groups receiving lutein showed an increase in MPOD. Graph depicts the response in a subject dosed at 10 mg/day.
Ensuring adequate nutrient intake
Intake of an adequate amount of essential eye nutrients, including vitamins C and E, zinc, macular carotenoids, and omega-3 fatty acids, is fundamental to eye health. These nutrients are not synthesized by the body and must be obtained from diet or by supplementation. (4,5,26,30)
A variety of foods can be sources of lutein, zeaxanthin, and omega-3 fatty acids.
Dietary sources of key eye nutrients
Unfortunately, many Americans do not obtain adequate nutrition through diet alone. (34) The foods associated with high levels of lutein and zeaxanthin are among the food groups showing the greatest gap in attainment of recommended intake. (34) More than 95% of adults have intakes of dark green vegetables, orange vegetables, and legumes that are below the minimum recommended amount. (34) Zinc intake is suboptimal, particularly in older people, with 20%-25% of the population aged 60 years or older not obtaining adequate daily zinc intake. (35)
On any given day, 75% of the US population does not consume any of the longer-chain omega-3 fatty acids, DHA or EPA. 30 Most omega-3 fatty acid intake is in the form of alpha-linolenic acid, of which only a small (≤15%) amount is converted to DHA and EPA. (33)
The major dietary source for DHA and EPA is fish; however, consumers need to be careful about which fish they eat and how often. Accumulation in the body of environmental contaminants such as methylmercury and polychlorinated biphenyls (PCBs) is a concern with frequent consumption of certain species of fish. (33)
Dietary supplementation
 For many individuals, dietary supplementation may be an option to help provide adequate nutrient intake. Conventional multivitamins contain little (0.25 mg) or no lutein. (36-38) However, nutritional supplements specifically formulated for eye health, with more lutein (5 mg), zeaxanthin, DHA, EPA, vitamins C and E, plus zinc, are available. The DHA and EPA in these nutritional supplements for the eye are sourced from smaller species of fish, such as anchovies, that do not accumulate toxins. (33)
For many individuals, dietary supplementation may be an option to help provide adequate nutrient intake. Conventional multivitamins contain little (0.25 mg) or no lutein. (36-38) However, nutritional supplements specifically formulated for eye health, with more lutein (5 mg), zeaxanthin, DHA, EPA, vitamins C and E, plus zinc, are available. The DHA and EPA in these nutritional supplements for the eye are sourced from smaller species of fish, such as anchovies, that do not accumulate toxins. (33)
Over half of adults use at least one dietary supplement, suggesting that awareness of the benefits of supplementation is high. (39) If patients are not asking about multivitamins for eye health, it may not be due to lack of interest. It may reflect a lack of knowledge about what options exist.
You would have to eat 4¼ cups of fresh broccoli every day to obtain a daily intake equivalent to 5 mg lutein.
Good nutrition and in some cases Neutraceutical supplements are the foundation of long-term eye health.
Measuring the levels of Antioxidants
Fight the war on cancer with prevention. Dr. Oz names the top 3 cancer fighters you need on your grocery list.
Ultraviolet (UV) light
Ultraviolet (UV) light is harmful to the eye and may lead to cataracts and age-related macular degeneration (AMD). Ultra-violet light is that portion of the spectrum of invisible light below 286nm to 400nm. UV light is divided into three segments, which are designated as A, B, and C. UVC (below 286nm) is effectively filtered by the earth’s ozone layer. UVB (286-320nm) is that solar energy which is the cause of sunburn and snow blindness and is absorbed by the cornea. UVA (320-400nm) is that part of the invisible spectrum of particular concern to eye care professionals. It is the most damaging of UV radiation and it is the radiation transmitted to the crystalline lens of the human eye.
Researchers have identified melanin as the substance in the skin, hair and eyes that absorbs harmful UV and blue light. It is the body’s natural sunscreen protection. Higher amounts of melanin afford greater protection against damaging light rays, but melanin is lost as we age. By age 65, about half of the protection is gone so that we are more susceptible to eye disease such as macular degeneration. of the spectrum.” Very bright lights such as sunlight or its reflection in the ocean or desert may cause damage to the macula.
Retinal damage is the most important hazard from light. The three types of retinal damage are structural, thermal and photochemical. The type of damage depends on the wavelength, power level and exposure time.
We advise patients to protect their eyes from potentially harmful UV light. Not only is harmful UV light present on sunny days, it is also present on overcast or hazy days. UV protection is available for clear lenses as well as sunglasses. The UV protection that is available is an invisible coating that doesn’t change the color of the eyeglass lens.
Misleading claims about certain glasses providing UV protection can be easily confusing to patients. A pair of glasses might be labeled UV-absorbent, for example, but the label might not indicate exactly how much UVA and UVB rays are blocked. Sunglasses should be labeled UV 400. It is recommended that you protect yourself from UV radiation up to 400 nanometers, which extends into part of the visible spectrum to ensure complete blockage of ultraviolet light. This is what distinguishes “cheap” sunglasses from more expensive ones. (1)
Patient Website Links
Fight the war on cancer with prevention. Dr. Oz names the top 3 cancer fighters you need on your grocery list.
Pharmanex Links
What does my scanner score mean?
Which Neutraceutical is right for me?
Eye Formula
NanoPak
Marine Omega
Science behind Pharmanex products
ARMD Links
www.PreventMacularDegeneration.org
http://www.nei.nih.gov/amd/
Sequenom Links
http://www.sequenomcmm.com/amd/
http://www.sequenomcmm.com/home/patient/amd/
References
- Beatty S, Koh H, Phil M, Henson D, Boulton M. The role of oxidative stress in the pathogenesis of age-related macular degeneration. Surv Ophthalmol. 2000;45(2):115-134.
- Trieschmann M, Beatty S, Nolan JM, et al. Changes in macular pigment optical density and serum concentrations of its constituent carotenoids following supplemental lutein and zeaxanthin: the LUNA study. Exp Eye Res. 2007;84(4):718-728.
- Whitehead AJ, Mares JA, Danis RP. Macular pigment: a review of current knowledge. Arch Ophthalmol. 2006;124(7):1038-1045.
- Grahn BH, Paterson PG, Gottschall-Pass K, Zhang Z. Zinc and the eye. J Am Coll Nutr. 2001;20(2):106-118.
- Liebovitz BE, Siegel BV. Aspects of free radical reactions in biological systems: aging. J Gerontol. 1980:35(1):45-56.
- Burton GW, Traber MG. Vitamin E: antioxidant activity, biokinetics, and bioavailability. Annu Rev Nutr. 1990;10:357-382.
- Cho E, Hung S, Willett WC, et al. Prospective study of dietary fat and the risk of age-related macular degeneration. Am J Clin Nutr. 2001;73(2):209-218.
- Chong EW-T, Kreis AJ, Wong TY, Simpson JA, Guymer RH. Dietary omega-3 fatty acid and fish intake in the primary prevention of age-related macular degeneration. Arch Ophthalmol. 2008;126(6):826-833.
- European Food Safety Authority. Scientific opinion on the substantiation of health claims related to docosahexaenoic acid (DHA) and maintenance of normal (fasting) blood concentrations of triglycerides (ID 533, 691, 3150), protection of blood lipids from oxidative damage (ID 630), contribution to the maintenance or achievement of a normal body weight (ID 629), brain, eye and nerve development (ID 627, 689, 704, 742, 3148, 3151), maintenance of normal brain function (ID 565, 626, 631, 689, 690, 704, 742, 3148, 3151), maintenance of normal vision (ID 627, 632, 743, 3149) and maintenance of normal spermatozoa motility (ID 628) pursuant to Article 13(1) of Regulation (EC) No 1924/2006. EFSA Journal. 2010;8(10):1734.
- Bazan NG. Homeostatic regulation of photoreceptor cell integrity: significance of the potent mediator neuroprotectin D1 biosynthesized from docosahexaenoic acid: the Proctor Lecture. Invest Ophthalmol Vis Sci. 2007;48(11):4866-4881.
- Johnson EJ, Chung H-Y, Caldarella SM, Snodderly DM. The influence of supplemental lutein and docosahexaenoic acid on serum, lipoproteins, and macular pigmentation. Am J Clin Nutr. 2008;87(5):1521-1529.
- SanGiovanni JP, Chew EY. The role of omega-3 long-chain polyunsaturated fatty acids in health and disease of the retina. Prog Retin Eye Res. 2005;24(1):87-138.
- Bone RA, Landrum JT, Guerra LH, Ruiz CA. Lutein and zeaxanthin dietary supplements raise macular pigment density and serum concentrations of these carotenoids in humans. J Nutr. 2003;133(4):992-998.
- Stringham JM, Hammond BR. Macular pigment and visual performance under glare conditions. Optom Vis Sci. 2008;85(2):82-88.
- Nolan JM, Kenny R, O’Regan C, et al. Macular pigment optical density in an ageing Irish population: the Irish Longitudinal Study of Ageing. Ophthalmic Res. 2010;44(2):131-139.
- Nolan JM, Stack J, O’Donovan O, Loane E, Beatty S. Risk factors for age-related maculopathy are associated with a relative lack of macular pigment. Exp Eye Res. 2007;84(1):61-74.
- Cai J, Nelson KC, Wu M, Sternberg P Jr, Jones DP. Oxidative damage and protection in the RPE. Prog Retin Eye Res. 2000;19(2):205-221.
- Liles MR, Newsome DA, Oliver PD. Antioxidant enzymes in the aging human retinal pigment epithelium. Arch Ophthalmol. 1991;109(9):1285-1288.
- Wyszynski RE, Bruner WE, Cano DB, Morgan KM, Davis CB, Sternberg P. A donor-age-dependent change in the activity of alpha-Mannosidase in human cultured RPE cells. Invest Ophthalmol Vis Sci. 1989;30(11):2341-2347.
- Hammond BR Jr, Fuld K, Snodderly DM. Iris color and macular pigment optical density. Exp Eye Res. 1996;62(3):293-297.
- Ciulla TA, Curran-Celantano J, Cooper DA, et al. Macular pigment optical density in a midwestern sample. Ophthalmology. 2001;108(4):730-737.
- Loane E, McKay GJ, Nolan JM, Beatty S. Apoliproprotein E genotype is associated with macular pigment optical density. Invest Ophthalmol Vis Sci. 2010;51(5):2636-2643.
- Hammond BR Jr, Johnson EJ, Russell RM, et al. Dietary modification of human macular pigment density. Invest Ophthalmol Vis Sci. 1997;38(9):1795-1801.
- Johnson EJ, Hammond BR, Yeum KJ, et al. Relation among serum and tissue concentrations of lutein and zeaxanthin and macular pigment density. Am J Clin Nutr. 2000;71(6):1555-1562.
- Kopsell DA, Lefsrud MG, Kopsell DE, et al. Spinach cultigen variation for tissue carotenoid concentrations influences human serum carotenoid levels and macular pigment optical density following a 12-week dietary intervention. J Agric Food Chem. 2006;54(21):7998-8005.
- Wenzel AJ, Gerweck C, Barbato D, et al. A 12-wk egg intervention increases serum zeaxanthin and macular pigment optical density in women. J Nutr. 2006;136(10):2568-2573.
- Bone RA, Landrum JT. Dose-dependent response of serum lutein and macular pigment optical density to supplementation with lutein esters. Arch Biochem Biophys. 2010;504(1):50-55.
- Rodriguez-Carmona M, Kvansakul J, Harlow JA, et al. The effects of supplementation with lutein and/or zeaxanthin on human macular pigment density and colour vision. Ophthalmic Physiol Opt. 2006;26(2):137-147.
- Schalch W, Cohn W, Barker FM, et al. Xanthophyll accumulation in the human retina during supplementation with lutein or zeaxanthin—the LUXEA (LUtein Xanthophyll Eye Accumulation) study. Arch Biochem Biophys. 2007;458(2):128-135.
- Office of Dietary Supplements, National Institutes of Health. Omega-3 fatty acids and health. http://ods.od.nih.gov/factsheets/OmegaFattyAcidsandHealth/. Accessed August 6, 2011.
- Perry A, Rasmussen H, Johnson EJ. Xanthophyll (lutein, zeaxanthin) content in fruits, vegetables and corn and egg products. Journal of Food Composition and Analysis. 2009;22:9-15.
- Thurnham DI. Macular zeaxanthins and lutein—a review of dietary sources and bioavailability and some relationships with macular pigment optical density and age-related macular disease. Nutr Res Rev. 2007;20(2):163-179.
- Kris-Etherton PM, Harris WS, Appel LJ, American Heart Association, Nutrition Committee. Fish consumption, fish oil, omega-3 fatty acids, and cardiovascular disease. Circulation. 2002;106(21):2747-2757.
- Krebs-Smith SM, Guenther PM, Subar AF, Kirkpatrick SI, Dodd KW. Americans do not meet federal dietary recommendations. J Nutr. 2010;140(10):1832-1838.
- Office of Dietary Supplements, National Institutes of Health. Zinc. http://ods.od.nih.gov/factsheets/Zinc-HealthProfessional/. Accessed August 24, 2011.
- Centrum® Silver® Tablets. Product Labeling. Pfizer Consumer Healthcare. Madison, NJ.
- One A Day® Men’s 50+ Advantage. Bayer HealthCare LLC. Morristown, NJ .
- One A Day® Women’s 50+ Advantage. Bayer HealthCare LLC. Morristown, NJ.
- Gahche J, Bailey R, Burt V, et al. Dietary supplement use among US adults has increased since NHANES III (1988-1994). National Center for Health Statistics Data Brief. 2001;61.
Share This